The human heart is a complex and vital organ, responsible for pumping blood throughout our bodies. To do this effectively, the heart must remain in good health. However, there are many conditions that can affect the heart's functioning, one of which is non-infectious endocarditis. This is a type of inflammation that affects the endocardium, the inner lining of the heart.
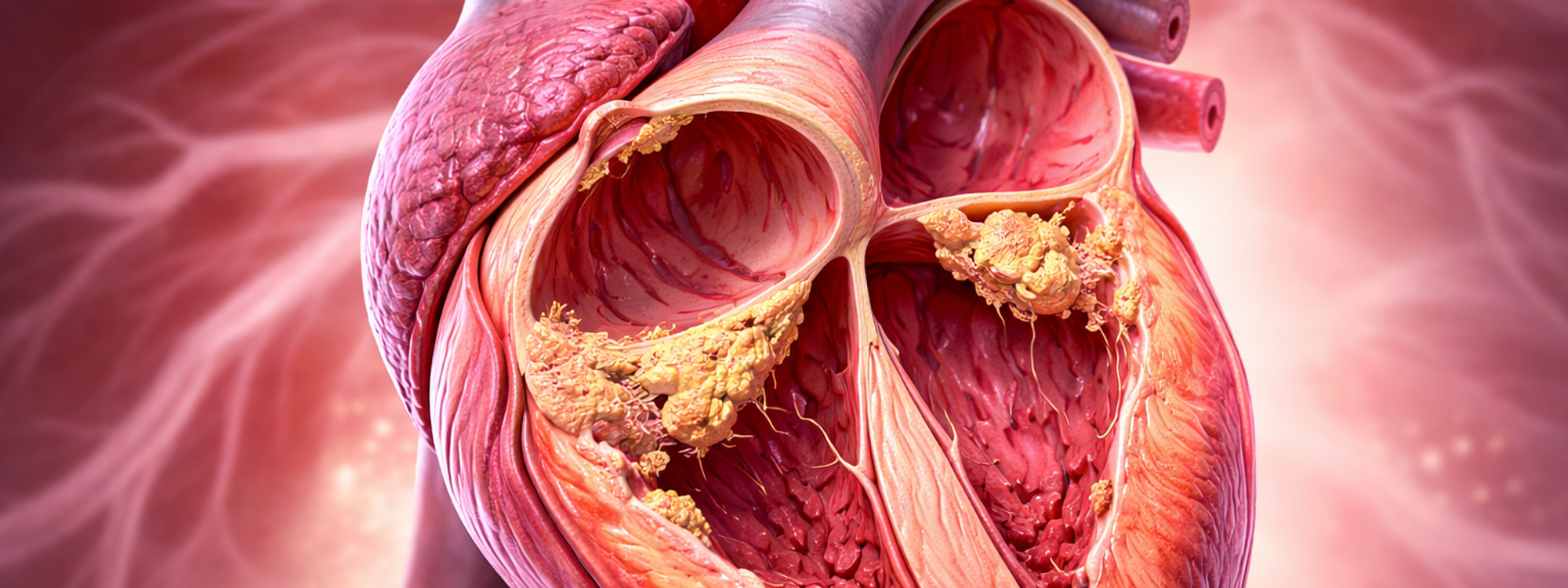
Non-infectious endocarditis, also known as aseptic endocarditis, is an inflammation of the endocardium. The endocardium is a thin, whitish membrane that lines the inside of the myocardium (heart muscle) and delineates the heart cavities.
The inflammation process in non-infectious endocarditis is characterized by the development of sterile platelet and fibrin thrombi. These are blood clots that form in response to various triggers, including physical trauma, local flow turbulence, the presence of circulating immune complexes, vasculitis (inflammation of blood vessels), and conditions that increase the blood's tendency to clot (hypercoagulable conditions).
Non-infectious endocarditis often develops on a heart valve that has been previously damaged, either by rheumatic fever or congenital heart disease.
The symptoms of non-infectious endocarditis are largely a result of arterial embolism, a condition where a blood clot blocks an artery. These symptoms can vary widely and include:
The sterile platelet and fibrin thrombi that characterize non-infectious endocarditis can damage valve function and worsen overall cardiac performance. Additionally, they can increase the risk of colonization by circulating microorganisms, potentially leading to infective endocarditis, a more serious condition.
Furthermore, the embolic phenomena associated with non-infectious endocarditis can affect other organs, including the brain, spleen, and kidneys.
The diagnosis of non-infectious endocarditis is typically suggested by negative blood cultures and confirmed by the results of an echocardiogram, an ultrasound of the heart.
Once diagnosed, treatment generally involves the use of anticoagulant medications, such as heparin or warfarin, to prevent further clot formation.