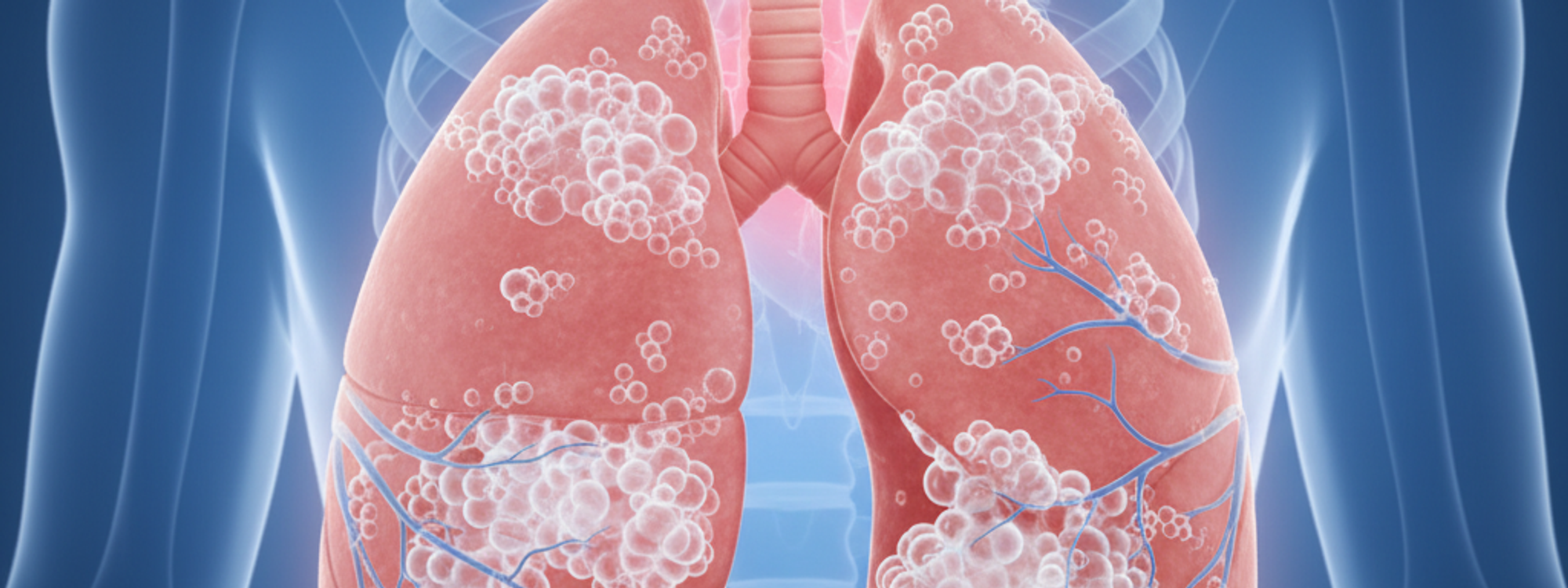
Pulmonary edema is a serious health condition that involves the accumulation of fluid in the lungs, specifically within the extravascular space. This accumulation of fluid can severely compromise the function of the alveoli, the tiny air sacs in the lungs where oxygen and carbon dioxide are exchanged. In severe cases, pulmonary edema can lead to respiratory failure.
The pathogenesis, or the biological mechanism that leads to the development of pulmonary edema, involves the transfer of fluid from the capillary system of the lungs into the interstitial spaces, and subsequently into the air cavities of bronchioles and alveoli.
The alveoli and pulmonary capillaries share a close relationship, separated only by a thin layer of cells. This proximity allows for the exchange of oxygen and carbon dioxide, a process that is critical for human breathing. When the alveoli are filled with fluid, their ability to facilitate this gas exchange is significantly hindered.
The fluid leakage can occur in two ways: through oozing, which is a result of increased pressure within the blood vessels, and through exudation, which happens when the vessel wall's permeability is compromised by an inflammatory process.
Pulmonary edema can be caused by a variety of factors and can be broadly classified into two categories: cardiogenic and non-cardiogenic.
Cardiogenic pulmonary edema originates from a heart anomaly such as hypertensive heart disease, ischemic heart disease, valvular diseases, congenital heart disease, or cardiac arrhythmias. These conditions affect the left half of the heart and are also referred to as left heart failure pathologies.
Non-cardiogenic pulmonary edema arises from different causes such as pulmonary veno-occlusive diseases, pulmonary vein hypertension, pneumothorax, pericardial diseases, liver disease, pneumonia, inhalation of toxic gases, high altitude, pulmonary embolism, opioid overdose, lymphatic carcinomas, allergic shock, eclampsia, and alterations in the permeability of the alveolar-capillary membrane.
Pulmonary edema is characterized by a set of symptoms that include difficulty breathing (dyspnea), excessive sweating, cyanotic coloration, dry cough, chest pain, heart palpitations, cardiac arrhythmias, hemoptysis, and hypertension. These symptoms can vary in severity depending on the extent of the fluid accumulation in the lungs.
Diagnosing pulmonary edema involves a combination of listening to the patient's lungs, chest x-ray, electrocardiogram (ECG), echocardiography, cardiac catheterization, pulmonary catheterization, and blood gas analysis. These diagnostic methods can help identify the presence of fluid in the lungs and shed light on the underlying cause of the condition.
The treatment approach for pulmonary edema is determined by the specific cause of the condition. However, generic therapy typically involves oxygen administration, intubation in cases of severe respiratory failure, and drug administration. Diuretics are often used to reduce fluid leakage into the interstitial space, and morphine may be administered to sedate the patient and aid in breathing.